When is chronic lymphocytic leukemia (CLL) in remission? What does it mean when the medical record states the CLL patient has a complete or partial remission? All great questions often heard around the table when cancer registrars get together.
CLL is the most common type of leukemia in the United States in American adults. Over 175,000 men and women are currently living with CLL, and many of them with a good quality of life. While a cure is not yet available there are a wide-range of effective treatments available today. For patients with slow-growing disease or who are in clinical remission, they may not even require active therapy. Of course, Cancer Registrars will be looking for all of this information and coding it appropriately in the case abstract.
Standard treatment for CLL is chemotherapy and radiation. However, newer treatments are being tested and made available to patients to help them achieve partial and complete remission for longer and longer periods of time. Newer therapies include:
- Immunotherapy:
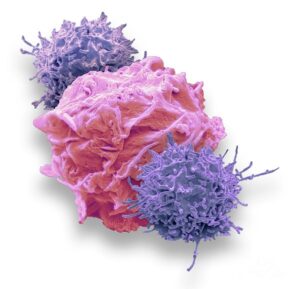
- Drugs that work with the body’s immune system to attack the cancer cells similar to how it attacks other diseases.
- Chemotherapy:
- Treatment regiments combined with stem cell transplant are being used to kill the cancerous cells in the body and are then replaced with healthy cells via a stem cell transplant.
- Targeted Drugs:
- These new medications attack specific substances that help the cancer cells to grow and multiply and leave the healthy, non-malignant cells alone.
There are two types CLL remission which we will describe below:
- Complete:
- If the patient’s blood tests no longer show the presence of CLL and they do not have any symptoms, such as swelling in the lymph nodes or spleen, then CLL is considered to be in complete remission.
- Partial:
- If the patient is symptom-free (i.e., no swelling in lymph nodes) but there is still a small amount of CLL detected in their blood tests, then they are considered to be in partial remission.
Laboratory tests are an important part of the medical record that the Cancer Registrar must review. For CLL you should look at the following:
- Blood Testing
- Diagnosing CLL usually starts with a routine blood test called complete blood count, or CBC. A CBC measures a number of different types of cells in the sample. For example, a patient may have CLL if the blood contains too many white blood cells, or WBCs. The CBC also measures red blood cells (RBCs) and platelets. Low levels of RBCs is called anemia and low platelet count is called thrombocytopenia.
- Flow Cytometry and Cytochemistry
- For these tests chemicals or dyes may be applied to the blood sample in the laboratory to provide information about the type and subtype of leukemia. CLL has distinctive markers, called cell surface proteins, on the outside of the cell. The pattern of these markers is called immunophenotype and is used to distinguish CLL from other types of leukemia that also involve lymphocytes. Flow cytometry, also called immunophenotyping, is the most important test used to confirm a diagnosis of CLL.
- Genomic and Molecular Testing
- These tests look for specific genes, proteins, chromosome changes or other factors unique to leukemia. Because CLL cells divide very slowly, looking at chromosomes is often less useful than tests that find specific genetic mutations or changes. Fluorescence in situ hybridization (or FISH) assays and other genetic tests, such as polymerase chain reaction, are used to find genetic mutations. Some of the genetic changes that are found in CLL include (but are not limited to):
- Deletion of the long arm of chromosome 13 [del(13q)], which is found in about half of all CLL patients,
- An extra copy of chromosome 12 (trisomy 12),
- del(11q),
- del(17p),
- NOTCH1 mutations,
- SF3B1 mutations,
- TP53 abnormalities,
- MYD88 mutations, and
- IGVH, which may be important whether it is changed or unchanged.
- Genomic and molecular testing can be used to determine how quickly the disease will progress and to identify treatment therapies and options. For example, if a patient has del(17p) genetic mutation then they are more likely to have a leukemia that is difficult to treat and some may work better than others.
- Imaging
- It is common for CLL to be found in many different parts of the body, even if diagnosed early. Imaging tests are rarely used to diagnose CLL but they may be used before treatment is given to identify areas of involvement or to determine how well CLL is responding to treatment.
- Bone Marrow Aspiration and Biopsy
- Bone marrow biopsy is also not generally used to diagnose CLL, but it may be done before treatment starts. It is useful to help determine the prognosis or a patient’s chance of recovery.
CLL can be in remission for many years, but there is always a chance it could come back. It is not uncommon for a physician to recommend a “watch and wait” form of long-term surveillance. This is why it is so important for the Cancer Registrar to understand the disease process and to gather accurate and complete follow-up and cancer status information throughout the patient’s lifetime.
Cancer Registrar’s should consult the SEER hematologic coding and abstracting resources to determine other steps or actions taken during the case abstraction process, whether they are in a SEER-designated State or not.
Disclaimer – this article is not used to determine coding or abstracting standrds! Rather it is an informational guide to help the Registrar understand what they may find in the medical record. For coding or abstracting standards please refer to your apppropriate manuals.